It was in 1981 at the age of 12 that Julia* noticed symptoms that scared her. When she used the toilet, and wiped with the toilet paper, she noticed blood in her stools.
Julia’s mother took her to emergency where she was admitted as a public patient and diagnosed with ulcerative colitis.
The initial treatment Julia received did not successfully address all the issues she was facing; at one stage she was given medication that made her so sick, she needed to be hospitalized. It was at that time Julia decided to seek out a private specialist, who diagnosed her condition as Crohn’s disease. Julia now understands that both conditions affect the bowel, but in slightly different ways, and the treatment for the two conditions may differ.
Julia is proactive in managing her condition with diet, exercise, and medication, and her symptoms are fairly well controlled. This is not always the case though, as she knows of many people who have Crohn’s disease and are in a lot of pain, and can’t work. Julia’s lifestyle is impacted as it is difficult for her to eat at restaurants and cafes. If Julia does eat out, which is rare, she will usually get abdominal pain and diarrhea, especially if she eats spicy food.
Julia sees her specialist every six months to get blood tests done to make sure all her markers are good. Julia understands that with Crohn’s disease, no matter how good her diet is, her body might not be absorbing the nutrient’s in the food she eats.
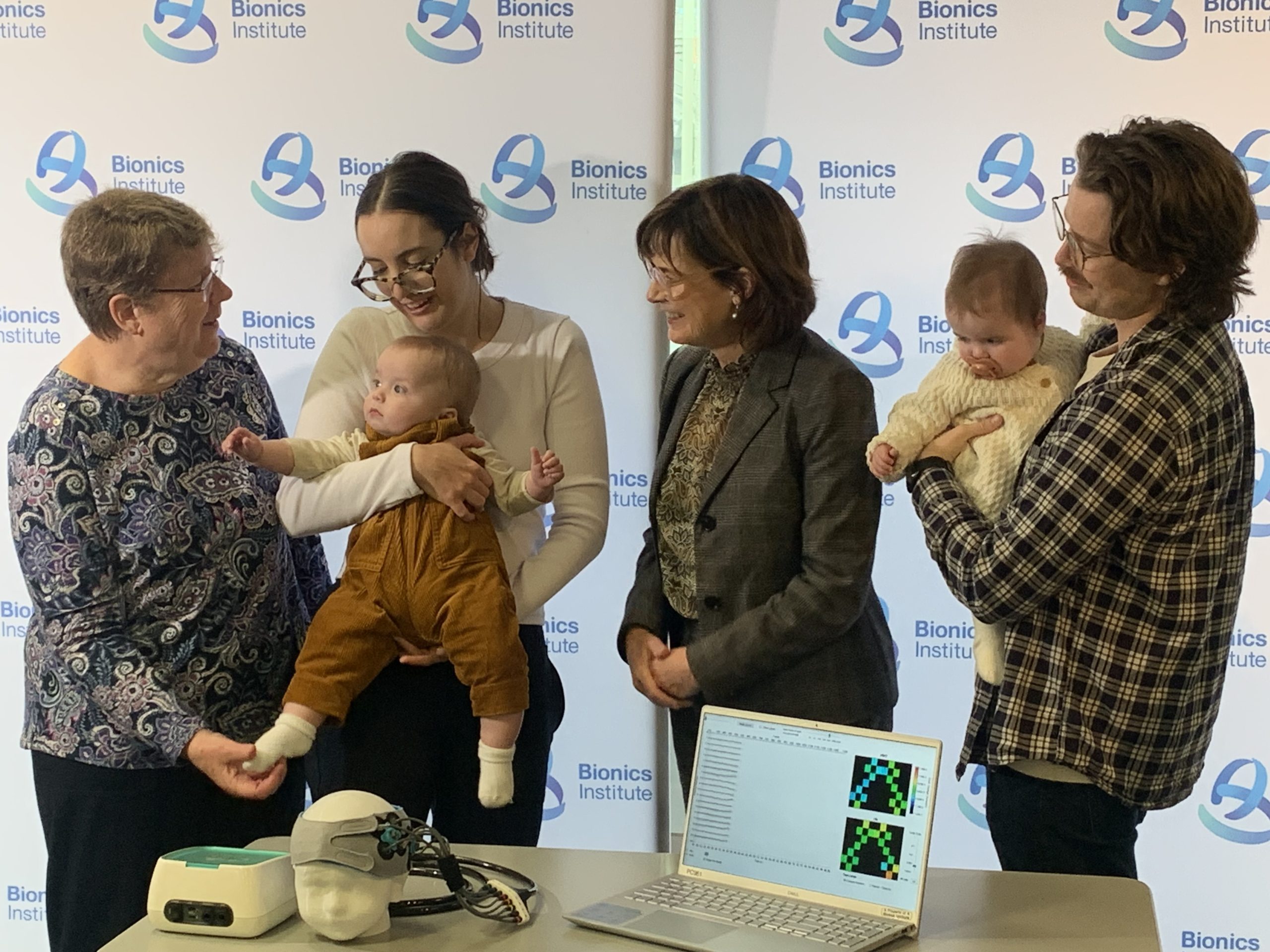
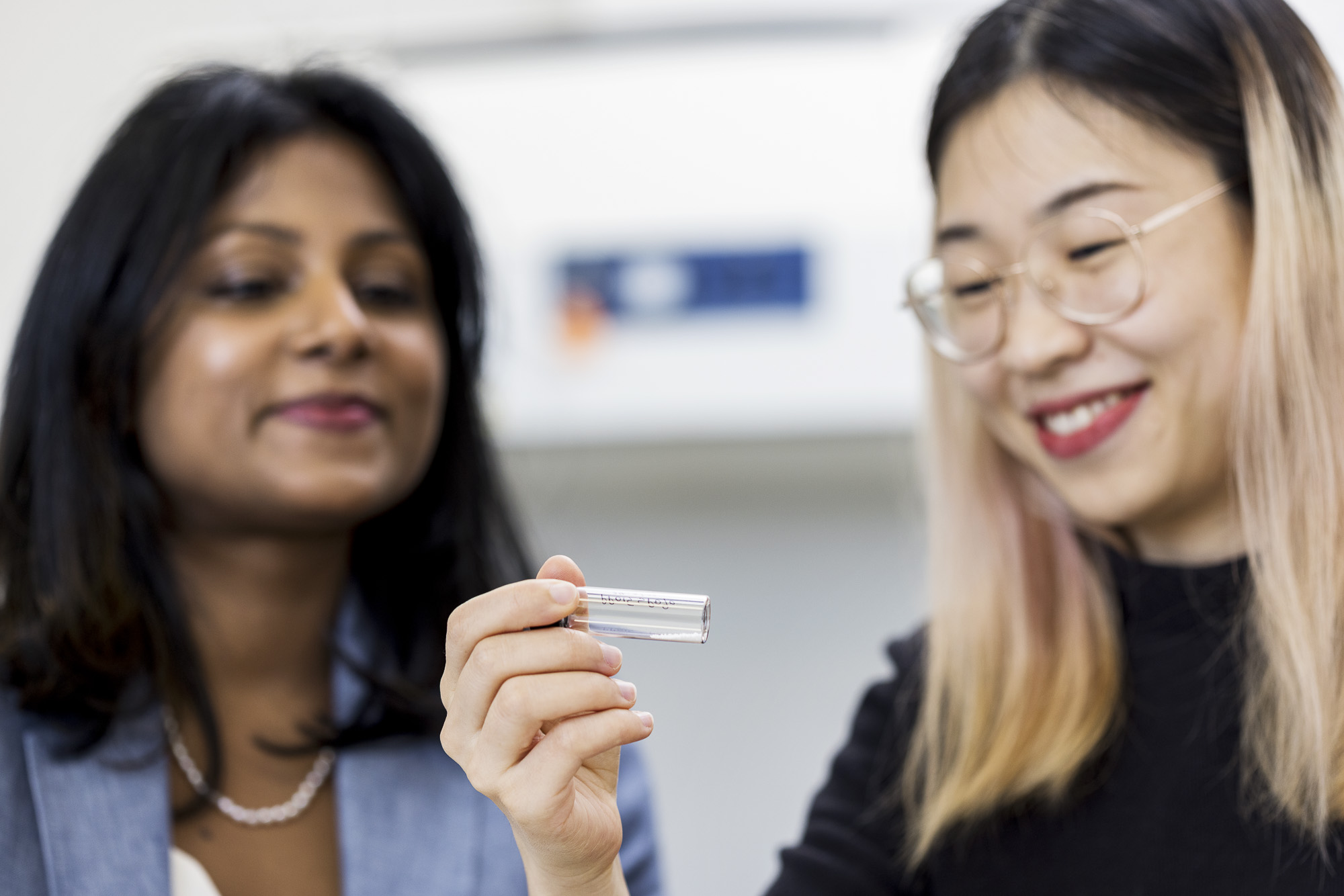
Julia believes any research into IBD is good research; she was very interested to read that our researchers have created a novel device that will enable detection of gut inflammation and will therapeutically stimulate the vagus nerve to ease the symptoms of Crohn’s disease.
*Julia is not this patient’s real name, who asked to remain anonymous. This is common with patients who suffer with IBD as many find it is a difficult topic to discuss.