Med Tech Talks
Innovating to prevent heart disease with Professor Karlheinz Peter
Professor Karlheinz Peter may have the solution that could save many lives.
Professor Peter and the team at Nirtek are developing intracoronary guidewire technology that can provide cardiologists with critical preventative health information.
When steered into the arteries of the heart, their device aims to use near infrared light to identify dangerous, rupture-prone plaques before they lead to heart attacks.
In this episode you will hear about:
More information:
Learn more about Professor Karlheinz Peter
Read some publications from Professor Peter
Learn more about Nirtek
Professor Karlheinz Peter [00:02:18] Thanks very much. It’s a pleasure for me to be here.
Robert Klupacs [00:02:20] It’s a great pleasure for you to give up your time, so I know how busy you are. We’ve got a few questions for you today and I know our listeners are going to be absolutely enthralled. First question for you. My researcher and I’ve done a bit of work on you and you’ve had a remarkable career. Can you tell our listeners what motivated you to become a cardiologist in the first place and how you landed in Australia via Germany and then the United States?
Professor Karlheinz Peter [00:02:45] Yeah, so it’s actually a very personal story. So I was at high school and I liked and was quite good in physics and chemistry, but I was a bit worried what the profession later on would be. And at that time I was reading a lot of physicists who developed weapons and I thought, oh, this is not a path that I would like to take. And then it happened that I was at home and my father developed chest pain and I just had my driver’s licence. So I drove him to the hospital and he had a heart attack there. And this was when I actually witnessed how much technology drives diagnosis and also therapy of heart attacks or heart diseases. And from that moment, I was really hooked to cardiology and I decided to study medicine, not going for physics. And very early on at medical school, I really put my effort in research. So I started in the physiology department, became assistant lecturer while I was still doing medical school. And often I sent friends of mine to sign in for me in the courses because I wanted to do my research projects. And then afterwards, after medical school, I looked around. So how do I combine medical work and clinical work with research? And to pass was to ask the GermanResearch Foundation for a training fellowship. And then I went to the US and that time molecular biology was in use;technology was cloning sequencing. So I went to the I studied that and I was lucky at Hopkins that a scientist who worked on acloned antiplatelet receptor took me in his lab and so I learned all the molecular biology, but I already had a topic that is very related to thrombosis and heart attack. And so that’s how I started in that area,then I went back to Heidelberg, which at that time was the top place really to get to training in cardiology. I finally got became Director of a cass lab in Freiburg. But then the situation developed a bit like, you know, the more advanced you get, the more clinical work you have to do, the more administration. And then the Baker offered me a position I didn’t actually plan, you know, to leave Germany. And, and this has the big advantage that I can do, you know, 75% research and 25% clinical work. So I can really focus on research.
Robert Klupacs [00:05:22] What a fantastic story. Looking at you in addition to all your clinical practice, all that training, you have made some quite amazing research impacts. I’ve read some of your papers, some of them I almost understand, and I’ll come back to Nirtek shortly. But one of your outstanding research outcomes has been the development of “intelligent drugs” The ideas of drugs being intelligent might actually surprise our listeners. So can you explain what these drugs are and how they can improve the lives of patients, particularly with cardiac disorders?
Professor Karlheinz Peter [00:05:55] Yeah, the term describes drugs that kind of work disease- specific, work localise where they are needed and don’t have side effects. So to give you an example, when you have antithrombotic drugs of analytic drugs, you don’t want to have bleeding. That’s a major complication and these drugs don’t do it. And the way how I started in this is a bit,as often in science, a complicated and not straightforward way. So when I started working on this receptor, I understood a bit how the receptor works – that it opens and signals. And then there was a new drug development coming up, which wasn’t at that time antibody drugs. So this was the third antibody drug ever developed. It was a huge commercial success for several years. It was the bestselling drug – it’s called IIb inhibitor. IIb for the receptor inhibitor because it blocks fibrinogen binding to the platelets and thereby clotting. And so this is a fantastic antithrombotic drug. It works when you have a heart attack; you inject it immediately and it protects more or less from further clotting. And then pharmaceutical – a nd this is actually quite interesting aspect from the commercialisation – pharmaceutical companies saw this principle and I think nearly 30 companies developed so-called super aspirin. So they thought, oh, if we block ligand binding to this receptor, then we have an oral aspirin, which is much more powerful. And so lots of money went into these companies and then we kind of, when the announcement was provided that this is a new strategy, I published a paper showing that if you imitate the ligand, then it binds to the receptor, then the receptor signals the platelet that it has to be activated. So it causes clotting. And so we got this really published with a lot of difficulties and then the situation was a bit that nobody really cited it because this was such a successful drug. And then the first trials came out and it turned out that actually patients got killed by this drug so the mortality was worse and then there was a big outcry and say, how can this be? And then suddenly our manuscript was published. And so we kind of described early on a mechanism that prevents this drug class. And it was, I think, up to nowadays people think it was the biggest pharmaceutical disaster financially because lots of companies went broke and the whole programs were stopped and this super aspirin was gone. But seeing this and then I thought, oh, there must be a way how to develop a drug that only blocks this activated receptor. And at that time a single chain… a technology was just developed. And I was lucky at the German Research Cancer Centre to get to know a person who just founded a small company, Affitech. At that moment Affimed and Affitech, these were the two companies. And so we designed a library, cloned the single chain antibody, and then we could show that this antibody actually blocks only activated platelets, doesn’t have any of these side effects and is very powerful. And so we went out to big pharmaceutical companies and we went in there we say, “oh, we have a new to be IIB blockers. And then even sometimes at the reception, they knew this was a disaster. And so we didn’t even get to suggest this new drug. So it failed because it was a toxic, target at the end. And so it was for me very interesting to see how the, you know, the pharmaceutical industry works. That you have kind of a target that has worked in one case and then like, you know, a sheep heard they all walk in one direction without thinking what they are doing. And that that was the basis of this new drug development. And we… because we couldn’t really make the point; we could show that it’s better, but nobody wanted to invest, you know, the millions necessary to develop this. And so we use this technology now to use the antibody as a delivery device. So it goes to activated platelets and we can provide fibrinolytics drugs to that spot. We can provide inflammatory drugs at site specific. And so it’s a very efficient system where we have now proof of concept in lots of animal models. And now we are in a stage that big pharmaceutical companies are interested and we collaborate with them and they do parts of the validation in animal models and we make sure that we have a strong patent coverage on that.
Robert Klupacs [00:10:51] And that’s how long before that new, that long-term developing drug delivery system is going to be in clinical trials.
Professor Karlheinz Peter [00:10:58] That’s ah… so we still have to get the, you know, the approval to fund this. And when you look, for example, to give you an idea, CSL has a drug for cardiovascular indications and they estimate it’s 1.5 billion AUD that they have to invest. So it has severe you know… I think even a company like CSL does not make these decisions too often. It’s quite a risky business. So it’s it shows you how expensive drug development is and especially in the cardiovascular area. And this is the bit… the problem of the field that we need. We already have good drugs and to show improvement we often need 15000 to 20000 patients to make, you know, to show that they work. And so when you look critically, there are not a lot of new developments because of this large hurdle.
Robert Klupacs [00:11:54] So is that reason that you decided to move into the device side, when you..I’m being a bit flippant, my listeners. A few years ago, Professor Peter and colleagues at Swinburne and the Baker Institute created a company called Nirtek to develop a particular type of technology,as I said in the beginning, to identify unstable plaques. I’m fascinated to know, for our listeners, why that’s so important, how you came up with it. And I think this sounds a little bit different to your drug development story because there were other types of people involved.
Professor Karlheinz Peter [00:12:28] The background is the same that we have this, you know, large group of patients who develop a heart attack, and it’s still the major cause of death and cardiovascular disease. Coronary artery disease kills probably it’s around 40 to 50% worldwide. So the numbers are huge. And when you look at countries like China or India, where they take up our probably bad lifestyle, it’s even getting worse in these countries. And so the finding that thrombosis is, you know, one approach. But this plaque targeting approach is a different one. So when you look at how an atherosclerotic plaque develops, you have the precision of calcium debris, all kind of dead cells, and then suddenly a plaque ruptures and then causes the clotting and the heart attack. And because the heart muscle is not perfused with blood anymore. And the frustration that we have as cardiologists, we when (as you mentioned), when we do an angiogram, we just see that in a lumen of a vessel. We don’t know what’s happening in the wall and we don’t have any technology available to predict whether someone has a plaque that ruptures or that is stable. And so when you come tomorrow and ask me to do a stress test, you know, a heart check-up and I’ll tell you, “you are all fine. There was no problem”. And the next day you come in with a huge heart attack and look in my eye and, you know, tell me that’s probably the worst doctor that Iever saw. And this is the situation that we face. So we don’t have a means to tell someone whether they have problematic plaques in their coronary arteries. And so this is a topic that I have worked on probably over 25 years now. One of the issues was that there is no animal model that reflects this kind of unstable plaques. And so we developed over quite a few years an animal model that has that one spot unstable plaque so we can really directly it to a specific spot. And then by chance, a student who probably didn’t really know what he was doing put this on a near-infrared camera and suddenly saw this thing lights up. And then he thought he did some mistake. And we we did it with another mouse and several mice. And it always did light up very strongly when we used a light in the area of 600 to 700 nanometres. So in the near infrared spectrum. And then we thought, “Oh, this is a mouse specific thing”. And we got some plaques from patients who had strokes and who also have these unstable plaques and it lights up as well. So we were quite surprised. Now we have something new and that’s when we got the patent. And I think that’s the real basis of the Nirtek company, because then we had this characteristic and knew we had something new that for the first time will be able to detect when you have a plaque at risk to cause a myocardial infarction, a heart attack. And then the the question was because light you can’t do a scanner technology because light doesn’t really go through the body. And so we had to be at the site where these plaques are. And we thought that we use a guide wire – shine light inside of the coronary arteries. And when we get this reflection that is specific, then we can say this is now an unstable plaque. And that’s the fantastic technology. It’s it’s the only technology that can do this reliably. We have lots of mouse data in the US. There was a group who tested a similar device and they also saw this in the coronary artery. So we have animal and as well as human proof. And now the company that we founded is really specifically, you know, kind of… it specifically aims to develop this guidewire with the best technology available and make it available to patients as soon as we can.
Robert Klupacs [00:16:29] How do you to develop that? So just thinking about the products. And most people, I think, are now aware of stenting. So is the idea that you would put a stent in and put a guidewire into the stent to be able to image whether or not there’s unstable plaques?
Professor Karlheinz Peter [00:16:42] So the idea would be when we have someone who comes with an infarct, who had one ruptured plaque already, that we would screen the other coronary arteries before stenting, or if someone comes with chest pain, we would also screen the coronary arteries. And then the advantage of the guidewire is that we can use this wire directly to place a stent there, so we don’t have to change anything. So it’s the fastest approach.
Robert Klupacs [00:17:06] Is the guidewire put in the same way as stents, just through the arm up the veins?
Professor Karlheinz Peter [00:17:10] So yeah it’s the same technology. So it’s very advanced, the technology. And that’s I think the advantage that we have is as a company that there are, you know, guidewire technologies around, so we have to adopt this for our specific purpose.
Robert Klupacs [00:17:25] It seems remarkably, you know, clever. You’re building on what’s already there. You’ve got technology to add to what’s being used routinely, but with greater… It sounds like a pretty simple pathway to development. I’m sure it’s not. Have you…can you just tell our listeners what the next steps are you need to do to get this to commercial reality?
Professor Karlheinz Peter [00:17:43] So we… I think the important thing is that we have people who drive this development within the company. So we were quite lucky to have, you know, the technical expertise but also the financial and the CEO expertise, so to say. And then with Neo-Bionica here, we also have a lot of the technical development expertise that we need, and that’s actually quite a fantastic situation. And we got a first investment by private investors but also by the government – the MRF Fund. So this is the federal government that saw the importance of this development. They gave us $750,000 also as part of the first investment. And we advance now that we have the first proof of concept in the technology and we hope that we soon have a kind of a prototype that we can test. And as always, you know, this costs a bit more money than we initially anticipated. So we have the money now to go on for a while, but we still need more funding to to bring the technology and the patients.
Robert Klupacs [00:18:57] And what would be a reasonable estimate to go from where you are today to get this in clinical proof of principle in, say, 50 patients to perhaps get FDA approval? Is it $5 million, $10 million, $20 million.
Professor Karlheinz Peter [00:19:09] Our estimate is now 7 million Australian dollars.
Robert Klupacs [00:19:12] So, I mean it’s not a lot of money.
Professor Karlheinz Peter [00:19:14] For I mean… for the number of patients where we can use this and what it would make a major difference here no doubt.
Robert Klupacs [00:19:21] And you could do the trials here in Melbourne.
Professor Karlheinz Peter [00:19:22] Yeah. So we can we have at the Alfred Hospital we have other hospitals who already agreed. So we at the moment we have a prototype we could get running.
Robert Klupacs [00:19:31] That’s amazing. So just on that journey, I mean, obviously you’ve been involved in drug companies in your career. You’re now a start-up company at the bank getting money in. What’s been the learnings for you in that process? You know, as now an interventional cardiologist, academic, researcher and now entrepreneur. Is there anything you’ve learnt that you sort of didn’t realise you had to know that? Yeah.
Professor Karlheinz Peter [00:19:56] So the the Baker is quite fortunate to have commercial support, you know, and the person that we have at the Baker is very knowledgeable and he’s very well connected in the entrepreneur space. So that was a big part of it. And then you need to find the right people in the company from the technical side, but also from the financial side. And I was actually quite surprised how complicated there area is and how difficult is it is to to find venture capital and especially in Australia. And so we I think at some stage we have to, you know, see for overseas investment as well.
Robert Klupacs [00:20:36] And it’s interesting because I think Australia clinical researchers have been around as well like you and they really are quite extraordinary, but not many clinical researchers that I’ve seen, have done what you’ve done and taken their technology and put in you’re a company for translation. Why do you think that is? And how do we get more clinical research like you because that’s where a lot of where the rubber hits the road actually in innovation. How do we get more of them involved in this process?
Professor Karlheinz Peter [00:21:03] Yeah. I mean one difficulty is that physicians often don’t have the time. They are so busy with clinical work. And so the having investment from the government in this space that physicians have a bit of time and that we have more funding in the basic research, I think will automatically create more of these opportunities. And then having, you know, this valley of death that we often see, that we have fantastic innovation, but then to develop it to a clinically usable product. And that’s a big gap. And I think currently what we see in Victoria with the Breakthrough Victoria, for example, that really goes in the right direction. And another area where we see that the government has seen the, you know, the signs of the future is the mRNA development. And I think that’s that’s also a very important investment and these areas are quite, quite important that we have state government investing. And another part which I personally witness often is that we have a more academic difference in how we score academic achievements so that we provide people the opportunity to go into a company for a few years and then go back to academia. Currently, that’s not possible because often it’s the end of their academic career and that’s in the US that it’s different. So you have people going into you into it as an entrepreneur and then they come back to academia and, and that I think being being able to move between the two sides is very important.
Robert Klupacs [00:22:47] I’m interested, you began your studies in Germany, as you said before, and workedand trained in the United States and now you’re in Australia. From your perspective, how does Australia compare to Europe, Germany and the United States from a STEM education point of view? Here we’re really passionate about the next generation of people getting into STEM. How do you think we compare?
Professor Karlheinz Peter [00:23:09] It’s an interesting question. The… so when you look at politics in Germany, you wouldn’t find a single party who doesn’t have a science portfolio and then they, you know, the population agrees that, you know, science is the only means how the country can be competitive on the international market. Australia is, as you say, a lucky country. And so we don’t need science really. And when you look at parties, it’s… for them it’s… people think if they come up with scientific topics, it’s rather an argument for voters not to vote for them. So you see that science is not part of political campaigns, and often we don’t have science ministries in the federal, state…. federal as well as state level. So the importance of science is being a part of modern society. I think that’s something politics has to work on. And the other part is that looking at gender equality in the STEM area, I think Germany has better laws in a way that, you know, you can have parental leave and its father and mother for longer time. And I think the politics has to, you know, to push for that. And I think the ideal for me, the ideal setting is that we have more women in STEM topics. And I think it gives the… it’s a healthier and more productive environment. At the Baker, for example, we try to achieve this was, you know, female fellowships and a special support program so that we, for example, if someone goes on maternity leave, we pay for a research assistant over a certain time. And so these are small measures, but I think they will make a big difference.
Robert Klupacs [00:24:58] And that’s a great insight. One of the other key themes of this podcast we’ve done, we’ve interviewed, I think now 12 or 13 people, and we was asking the same question and it comes back to mentorship. We’re very passionate about it. And one of the things we really noticed about you when we did the research on you, as we said in the beginning, 120 people have come through your hands with PhD or fellowship training. You obviously have a passion for it. What makes a good mentor in your eyes Karlheinz?
Professor Karlheinz Peter [00:25:27] Yeah. For me, it’s often the combination with being a supervisor and discussing with students or postdocs what are their career options and doing this in relation to their talent as well , because you can’t give everybody the same advice. And so I think for me, the proudest achievement of my career is really keeping up with a lot of my previous students and supporting them and seeing them how they advance academia and become successful there. I think that’s a big, big part of it.
Robert Klupacs [00:26:02] The other thing, what I’ve loved and I always ask this question to people:who was your mentor and who had the biggest impact on your career?
Professor Karlheinz Peter [00:26:09] Yeah, so that’s an interesting question. So obviously there are a lot of talented and driven people I had contact to, but I also realised that often because it was combined with being a supervisor that they had their own agenda as well. So I became a bit careful to discriminate between, you know, what is really the interest of myself and those of my career in comparison to the interest of the supervisor. And I think that’s an important part of being, you know, a mentor that you give the best advice, independent of your own advantage as a supervisor or mentor. And therefore, I think having a mentor that is a bit far further away from your own research and potentially not your supervisor is actually quite important; to have this independent advice. And I didn’t have a mentor like that because previously was always, you know, the supervisor role. And I think separating the two roles is quite important.
Robert Klupacs [00:27:13] Do you think in the Australian STEM community that we both work in, that there’s good mentorship or could we improve it?
Professor Karlheinz Peter [00:27:19] Yeah, I think the importance has been recognised and so most institutes have now mentor programs and that that actually works quite well.
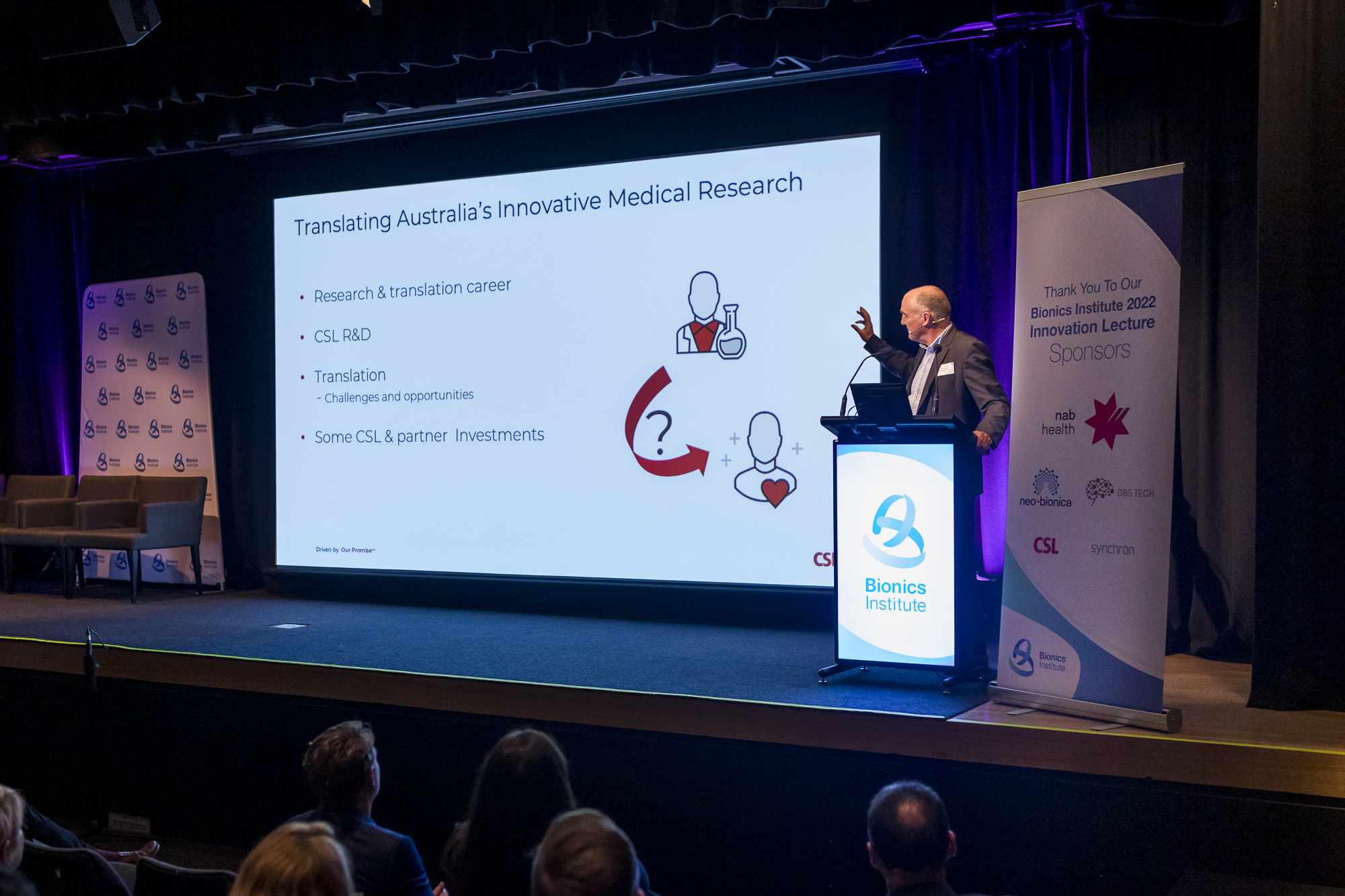
Robert Klupacs [00:27:29] Oh good. We’re reaching the end of the podcast, so I want to leave the biggest question for last and get your opinion on this. Despite having a very strong research and development sector in Australia. You mentioned the science before. Australia ranks 25th out of 132 economies in the Global Innovation Index, which we’re very proud of. But we’re only in the sixties for research translation – turning it into something. What do you think? You know, as a person who’s very clinically orientated, what do you think Australia should do to improve that performance of turning great academic capability into something that’s going to have clinical output?
Professor Karlheinz Peter [00:28:05] Yeah. So one of the major issues I think is funding through federal and state governments. And when you look at, you know, the percentage of GDP. I don’t want to argue with numbers, but when you compare to the US, Germany, Switzerland or France, you know, the percentage is much higher than in Australia. So the more funding and basic research you provide, the more new developments will show up. And then a big part of it is kind of having this specific translational seed funds, both in regards to projects, but also rooms – having these incubator areas like CSL and Uni Melbourne with the Victorian Government is doing this now is is quite important and also having potentially fellowships for people, you know, when they want to come back. As I mentioned before, from, from companies going into academia as well is an important part. And so this this funding situation, I think that’s really a big concern for many working in the field, even if you have a translational direction. And yeah, and that’s a big part of it is also that we recognise we are a small country. There’s not a lot of, you know, venture capital available. And so the international connections I think are quite important as well.
Robert Klupacs [00:29:31] Karlheinz, we’ve reached the end of the podcast today. Thank you so much for everything you’ve said and giving us your time and sharing your insights with us, and particularly that last thing about how we can make sure that this country supports the great things happening at the coalface and turning them into something. To our listeners. I hope you enjoyed listening and I look forward to introducing you to our guests in future podcasts. There are links to everything we talked about in the show notes and we look forward to welcoming you next time.

Professor Karlheinz Peter, Deputy Director of the Baker Institute at the Alfred Hospital; and Chief Medical Officer at med tech company, Nirtek
Listen to other episodes of Med Tech Talks here